Stage 1: Early Stage (Mild RA)
In Stage 1, rheumatoid arthritis is just beginning to develop. Inflammation starts in the synovial membrane—the lining of the joints—but there’s no damage to the bones or cartilage yet.
Although joint tissue is inflamed and swollen, symptoms are usually mild and can be easily overlooked, which can delay diagnosis. However, early detection is critical—starting treatment within the first 12 weeks can significantly improve long-term outcomes and may even lead to remission.
Inside the Joint:
- The synovium becomes inflamed and thickened
- Joint fluid may increase, causing mild swelling
- No visible bone or cartilage damage at this point
Common Symptoms of Stage 1:
- Mild joint pain, swelling, or stiffness (especially in the morning)
- Fatigue or low energy
- Discomfort in smaller joints such as fingers, wrists, or toes
- Stiffness often improves with movement
For example, if Stage 1 RA affects the hands, a person may feel stiffness and discomfort in the knuckles and finger joints.
Diagnosis Tools:
- X-rays may appear normal at this stage
- Blood tests can detect:
- Rheumatoid factor (RF)
- Anti-CCP antibodies
- Elevated inflammation markers like ESR or CRP
Why This Stage Matters:
This is the most critical window for early intervention. When RA is diagnosed and treated early, joint damage can often be prevented or slowed, and in some cases, remission is possible.
Stage 2: Moderate RA
The disease progresses beyond inflammation. The synovial tissue remains swollen, but now it starts to affect the cartilage, which cushions the bones inside the joints. Damage is still in the early stages, but the effects become more noticeable—and more disruptive.
At this stage, many people begin seeking medical help because pain, swelling, and joint limitations are harder to ignore.
What’s Happening Inside the Joint:
- Continued inflammation in the synovium
- Cartilage begins to break down
- Joint space may narrow due to swelling and fluid
- Bones may still appear unaffected, but damage is starting
Common Symptoms of Stage 2:
- More persistent pain and swelling in affected joints
- Stiffness lasts longer, even with movement
- Limited range of motion or trouble using the joint
- Increased fatigue and possible muscle weakness
- Joints may feel warm to the touch
You might notice difficulty opening jars, walking up stairs, or typing due to pain in your hands, knees, or feet.
Diagnosis Tools:
- X-rays may begin to show early signs of cartilage damage
- MRI or ultrasound can detect more subtle joint changes
- Blood markers (RF, anti-CCP, CRP, ESR) likely remain elevated
Why This Stage Matters:
This is when joint damage begins to become permanent. While still manageable with treatment, it’s important to adjust therapies to slow progression and preserve joint function.
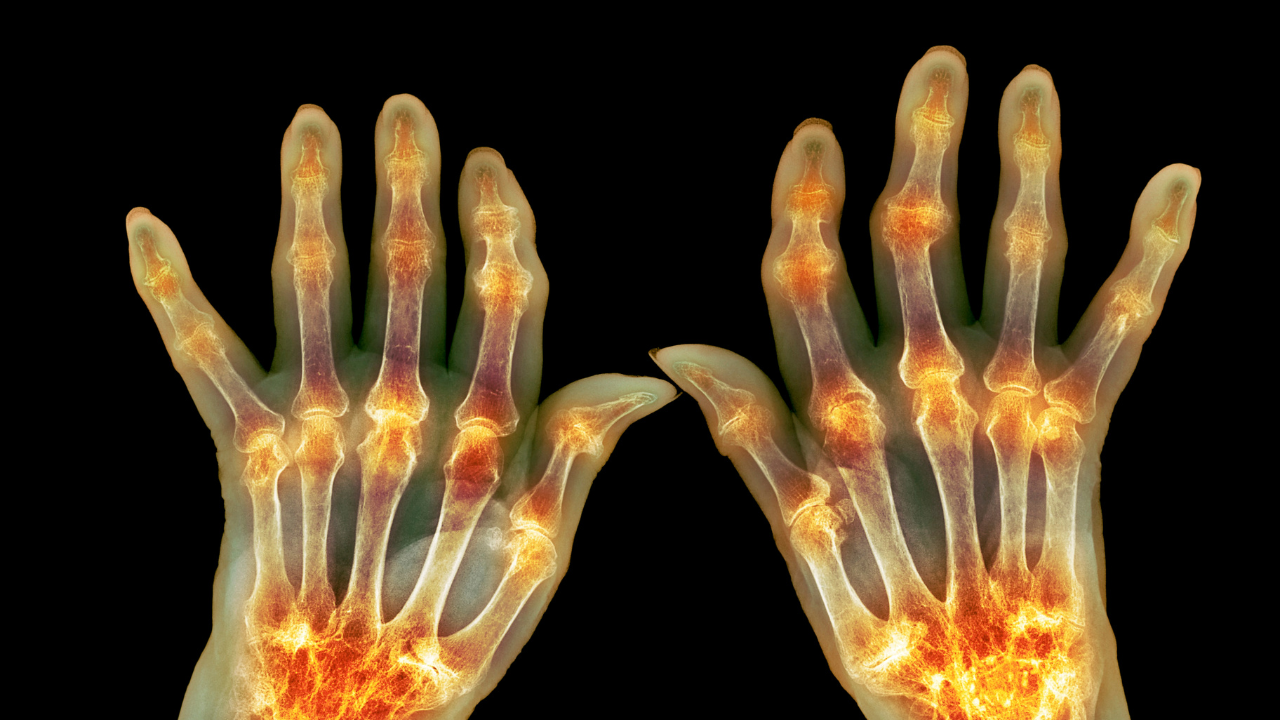
Stage 3: Severe Rheumatoid Arthritis
At Stage 3, also known as Severe RA, the disease becomes much more aggressive. Inflammation is no longer limited to the joint lining—it now starts to destroy cartilage and bone, leading to major joint damage.
What Happens in Stage 3?
- Erosion of cartilage and bones visible on X-rays
- Loss of joint space, increasing stiffness and immobility
- Formation of rheumatoid nodules around affected joints
- Visible deformities, especially in fingers, hands, and toes
Symptoms
- Intensified pain and swelling
- Significant loss of range of motion
- Fatigue and weakness
- Joint deformities that can interfere with basic tasks like gripping, walking, or dressing
Diagnosis Tools:
- X-rays show clear joint damage and bone erosion
- MRI or ultrasound can assess the full extent of damage
- Joint function tests may be used to determine mobility and strength
Treatment Options for Stage 3
By this stage, treatment becomes more intensive. Patients may already be using:
- Traditional DMARDs (like methotrexate)
- Biologic therapies (such as Humira, Enbrel, or Rituxan)
- Corticosteroids for inflammation control
- NSAIDs for pain and swelling
If these treatments fail to control symptoms, doctors may introduce:
- Janus kinase (JAK) inhibitors – A newer class of DMARDs that target specific inflammatory pathways (e.g., tofacitinib or baricitinib)
Managing Daily Life
- Assistive devices (braces, ergonomic tools)
- Physical & occupational therapy
- Joint protection techniques to reduce further damage
Early intervention is critical. Even in Stage 3, aggressive and consistent treatment can help slow further joint damage and improve quality of life.
Stage 4: End-Stage Rheumatoid Arthritis
In the final stage of RA, known as End-Stage RA, inflammation within the joints may decrease—but the damage is already extensive. At this point, joint function is often severely compromised.
What Happens in Stage 4?
- Joint destruction becomes irreversible
- Cartilage and bone loss is evident on imaging tests
- Severe pain, stiffness, and swelling may persist
- Joint deformities and loss of mobility are common
- Individuals often struggle with basic tasks, such as walking, dressing, or gripping
Symptoms
While inflammation may not be as intense as in earlier stages, symptoms are usually:
- More chronic and disabling
- Accompanied by significant loss of function
- Emotionally distressing due to physical limitations and loss of independence
Diagnosis Tools:
- X-rays or MRIs show full joint damage, erosion, or fusion
- Physical assessments show little or no joint range of motion
- Functional evaluations assess the impact on daily living
Treatment Options at This Stage
At this point, many people have already tried all available medical treatments. Remaining strategies may include:
- Surgery, such as:
- Joint replacement (arthroplasty)
- Joint fusion (arthrodesis)
- Synovectomy (removal of inflamed joint lining)
- Assistive devices, including:
- Walkers or canes
- Orthopedic shoes or braces
- Adaptive tools for self-care
- Physical therapy to maintain remaining function
- Occupational therapy for daily activity adaptations
- Pain management, including advanced medications and palliative care support
While end-stage RA can be life-altering, it doesn’t have to be life-limiting. With a personalized care plan and support system, many individuals continue to live with dignity and purpose.
Related Posts:
- what-are-rheumatoid-arthritis-and-osteoarthritis/
- What Is Rheumatoid Arthritis? Causes, Symptoms and Diagnosis
- Early Warning Signs of Rheumatoid Arthritis You Shouldn’t Ignore
How to Prevent Rheumatoid Arthritis Progression
While there’s no cure for rheumatoid arthritis, certain lifestyle changes and self-care strategies can slow the progression of the disease and improve overall quality of life. Everyone’s experience with RA is different, but these proven tips can make a meaningful impact:
Eat an Anti-Inflammatory Diet
A balanced, nutritious diet rich in:
- Fruits & vegetables
- Whole grains
- Lean proteins (like fish, legumes)
- Healthy fats (like olive oil and avocados)
- can reduce inflammation and support joint health.
Maintain a Healthy Weight
Excess weight puts stress on joints and may worsen inflammation. Achieving and maintaining a moderate weight can help improve mobility and reduce flare-ups.
Quit Smoking
Smoking is a known risk factor for developing and worsening RA. Quitting can help manage symptoms and improve your response to medications.
Stay Physically Active
Movement keeps joints flexible and muscles strong. Aim for:
- 150 minutes/week of low-impact exercise like:
- Swimming
- Cycling
- Walking
- Take daily movement breaks and limit prolonged sitting.
Rest & Manage Flares
During flare-ups:
- Rest often to preserve energy.
- Use heating pads or take warm baths to relieve stiffness.
- Try cold packs for 20-minute intervals to reduce swelling.
Try Natural Remedies & Topicals
- Use over-the-counter (OTC) pain-relief creams and patches.
- Consider topical NSAIDs as prescribed.
- Supplements like:
- Omega-3 fish oil
- Turmeric
- Gamma-linolenic acid (GLA)
- may help reduce inflammation (check with your doctor first).
Manage Stress
Chronic stress can worsen RA symptoms. Try:
- Deep breathing & meditation
- Guided imagery
- Gentle yoga or stretching
Stay Connected & Engaged
- Stay involved with friends, family, and hobbies.
- Don’t hesitate to ask for help during tough days.
- Join support groups or self-management education programs to learn coping strategies and connect with a community.
Consistency is key. By committing to these habits, many people with RA experience fewer flare-ups, better mobility, and improved emotional well-being.
Key Takeaways:
- Don’t ignore early signs, such as joint stiffness or fatigue—early diagnosis is crucial.
- Stay active, maintain a healthy weight, and follow your doctor’s treatment plan.
- Use assistive tools, embrace lifestyle modifications, and prioritize mental well-being.
RA may not have a cure, but with knowledge, support, and treatment, you can still live a full, empowered life.
Related Posts:
- what-are-rheumatoid-arthritis-and-osteoarthritis/
- What Is Rheumatoid Arthritis? Causes, Symptoms and Diagnosis
- Early Warning Signs of Rheumatoid Arthritis You Shouldn’t Ignore