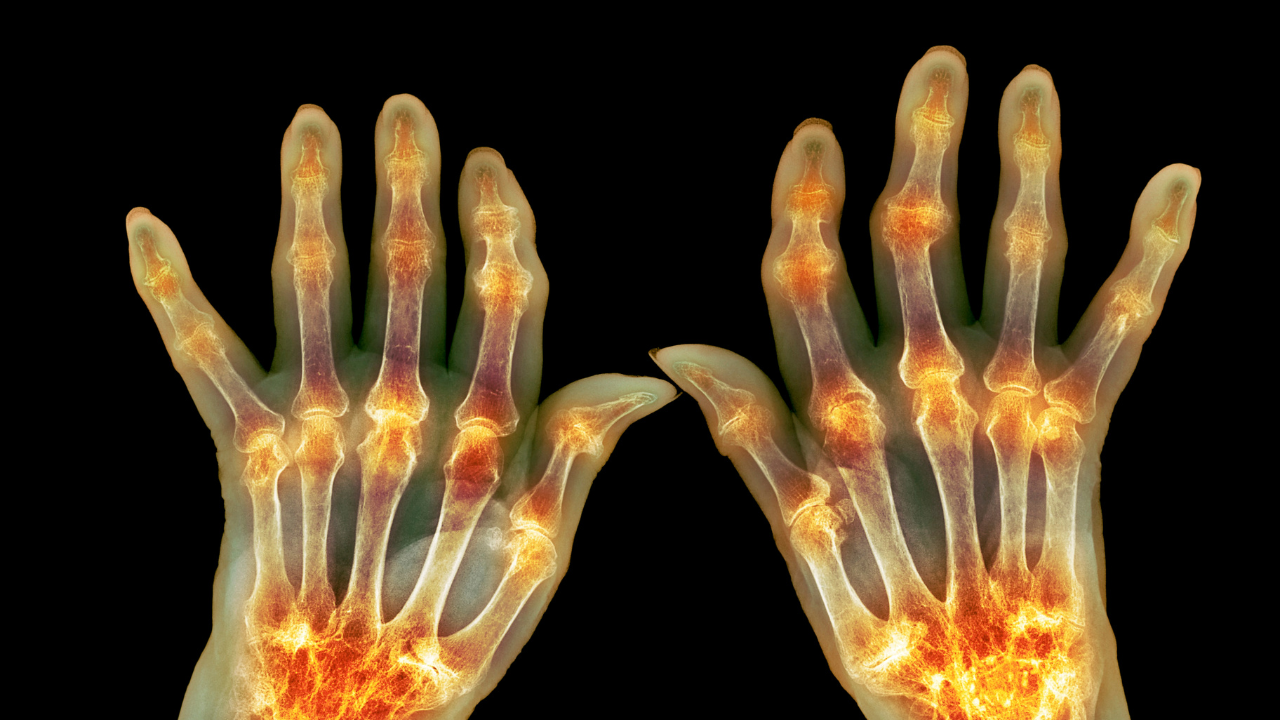
Rheumatoid arthritis (RA) and osteoarthritis (OA) are two of the most common forms of arthritis. While both conditions involve joint pain and damage, they are fundamentally different diseases, with distinct causes, symptoms, and treatments.
Rheumatoid Arthritis (RA) – An Autoimmune Condition
RA is an autoimmune disease, meaning the body’s immune system mistakenly attacks its own tissues. Instead of fighting off viruses and bacteria, the immune system begins to attack the synovial membrane—the thin lining that lubricates and protects your joints.
This leads to inflammation, swelling, and joint damage that can become progressively worse over time. RA often affects joints on both sides of the body (symmetrically) and can also harm other organs, such as the heart, lungs, or eyes.
Osteoarthritis (OA) – A Degenerative Joint Disease
OA is not an autoimmune disease. Instead, it’s a mechanical problem caused by wear and tear over time. It happens when the cartilage, the spongy material that cushions the ends of bones in a joint, gradually wears away.
As cartilage breaks down:
- Bones may rub against each other
- Joints become stiff, painful, or lose mobility
- The bone may develop bony spurs or thicken
OA usually affects weight-bearing joints like the knees, hips, and spine and often develops on one side of the body more than the other.
Key Differences Between RA and OA
| Feature | Rheumatoid Arthritis (RA) | Osteoarthritis (OA) |
| Cause | Autoimmune reaction | Wear and tear on joints |
| Onset Age | It can occur at any age | Typically, later in life |
| Speed of Onset | Rapid or gradual | Gradual |
| Joint Pattern | Symmetrical (both sides) | Often asymmetrical |
| Inflammation | Severe | Mild to moderate |
| Morning Stiffness | Lasts > 30 minutes | Usually < 30 minutes |
| Systemic Symptoms | Fatigue, fever, malaise | Rare |
| Joint Deformity | Common if untreated | Rare |
Why It Matters
Understanding whether you have RA or OA is crucial because treatment plans are very different. RA often requires immune-suppressing medications, while OA is typically managed with pain relief, lifestyle changes, and joint support strategies.
Summary
While RA and OA may both cause joint pain, their causes, progression, and treatment are quite different. If you’re experiencing symptoms like persistent joint pain, stiffness, or swelling, especially if it lasts more than a few weeks, consult a healthcare provider. Receiving the correct diagnosis early can make a significant difference in how you feel and move.
RA vs. OA – Understanding the Causes
Although Rheumatoid Arthritis (RA) and Osteoarthritis (OA) both affect the joints, they stem from very different underlying causes. Understanding what triggers each condition can help guide prevention, diagnosis, and treatment.
Osteoarthritis (OA) – Wear and Tear
Cause:
OA develops when the protective cartilage that cushions the ends of bones gradually wears down over time.
Common Causes and Risk Factors:
-
Aging: The natural wear and tear of joints with age is the most common cause.
-
Joint Overuse: Repetitive movements from certain jobs or sports can increase stress on joints.
-
Injuries: Past joint injuries, especially those that did not heal properly, can increase the risk of developing OA later in life.
-
Genetics: A hereditary tendency to cartilage deterioration may run in families.
-
Obesity: Extra weight puts more pressure on joints, especially the knees, hips, and spine.
Rheumatoid Arthritis (RA) – Autoimmune Attack
Cause:
RA is an autoimmune disorder, meaning the immune system mistakenly attacks healthy joint tissue, particularly the synovial membrane—the lining that protects and lubricates joints.
Common Risk Factors:
-
Genetics: Certain genes (e.g., HLA-DR4, PTPN22) are linked to an increased risk.
-
Environmental Triggers: Possible triggers include viruses, bacteria, or toxic exposures like asbestos or silica.
-
Hormones: RA affects women more than men, suggesting a hormonal influence.
-
Smoking: One of the strongest lifestyle risk factors for RA.
-
Obesity may worsen inflammation and increase the risk, especially in women under 55.
Important: While OA is primarily mechanical and degenerative, RA is inflammatory and systemic, potentially affecting the entire body.
Summary Table – RA vs. OA Causes
| Cause/Risk Factor | Rheumatoid Arthritis (RA) | Osteoarthritis (OA) |
|---|---|---|
| Main Cause | Autoimmune reaction | Cartilage wear and tear |
| Genetic Influence | Yes (autoimmune gene markers) | Yes (cartilage degeneration) |
| Environmental Factors | Smoking, toxins, infections | Joint overuse, physical strain |
| Hormonal Role | Yes – more common in women | No clear hormonal link |
| Injury History | May contribute indirectly | Direct link to old or unhealed injuries |
| Obesity | Increases risk and severity | Increases joint stress and OA risk |
Osteoarthritis vs. Rheumatoid Arthritis: Symptoms at a Glance
When visiting a doctor for joint pain, the location, pattern, and timing of your symptoms can provide important clues. Though both RA and OA affect the joints, the way they show up in your body is quite different.
Rheumatoid Arthritis (RA) Symptoms
RA is a systemic autoimmune disease that causes inflammation in multiple joints—and can affect the entire body.
Key symptoms of RA:
-
Morning stiffness lasting an hour or more
-
Symmetrical joint pain (both sides of the body—e.g., both hands, both knees)
-
Rapid onset and progression
-
Fatigue and low energy
-
Low-grade fevers
-
Loss of appetite
-
Joint deformities over time (joints may become stuck in bent positions)
-
Rheumatoid nodules (small lumps under the skin, especially near elbows or fingers)
RA can begin at any age, but most often appears in midlife.
🦴 Osteoarthritis (OA) Symptoms
OA is a degenerative joint disease caused by wear and tear on the joints. It develops gradually, most often in older adults.
Key symptoms of OA:
-
Joint pain that worsens with activity and improves with rest
-
Brief morning stiffness (usually less than 30 minutes)
-
Stiffness returns after periods of inactivity
-
Cracking or grinding sounds (crepitus) when moving the joint
-
Swelling—typically mild compared to RA
-
Joint instability or weakness
-
Usually affects one joint or one side of the body at a time
OA often targets weight-bearing joints such as the knees, hips, and spine.
RA vs. OA Symptoms – Quick Comparison Table
| Symptom | Rheumatoid Arthritis (RA) | Osteoarthritis (OA) |
|---|---|---|
| Onset | Can develop quickly | Develops slowly over the years |
| Age of Onset | Any age (commonly midlife) | Most common in older adults |
| Joint Pattern | Symmetrical (both sides of the body) | Often asymmetrical, one or a few joints |
| Morning Stiffness | Lasts ≥ 1 hour | Lasts < 30 minutes |
| Pain Pattern | Better with movement, worse in the morning | Worse with activity, better with rest |
| Swelling | Moderate to severe | Mild to moderate |
| Systemic Symptoms | Yes – fatigue, fever, appetite loss | Rare |
| Joint Deformity | Common if untreated | Rare |
| Cracking/Grinding (Crepitus) | Uncommon | Common |
| Rheumatoid Nodules | Possible | Uncommon |
Summary
Understanding the differences in symptoms between RA and OA is key to getting the correct diagnosis and treatment. RA is an inflammatory, fast-moving condition that affects the whole body, while OA is a mechanical, slow-developing condition that is more localized.
If you’re dealing with persistent joint pain or stiffness, especially if it interferes with your daily life, talk to a healthcare provider. Early detection and the proper care plan can greatly improve your quality of life.
Diagnosis: OA vs. RA
If you’re experiencing persistent joint pain, stiffness, or swelling, it’s essential to consult your healthcare provider. They can help determine whether your symptoms are due to osteoarthritis (OA), rheumatoid arthritis (RA), or another condition entirely.
How Are OA and RA Diagnosed?
The diagnostic process for both OA and RA involves several overlapping steps, including:
1. Medical History and Physical Examination
Your provider will:
-
Ask detailed questions about your symptoms, their duration, and which joints are affected.
-
Perform a physical exam to check for joint tenderness, swelling, range of motion, and visible deformities.
2. Imaging Tests
X-rays are commonly used for both RA and OA to:
-
Detect joint damage, cartilage loss, bone changes, or erosions
-
Show narrowing of joint space (typical of OA)
-
Identify bone erosions and soft tissue swelling (common in RA)
MRI or ultrasound may also be used in early or complex cases to assess soft tissue and joint inflammation.
3. Arthrocentesis (Joint Aspiration)
This procedure involves:
-
Drawing fluid from a swollen joint with a sterile needle
-
Analyzing the joint fluid for signs of:
-
Infection
-
Gout crystals
-
Inflammatory markers
-
This can help differentiate RA from OA or rule out other types of arthritis.
-
4. Laboratory Tests for RA
While blood tests cannot diagnose OA, they can be extremely helpful in identifying or ruling out RA or other autoimmune conditions.
Standard RA-related blood tests:
-
Rheumatoid Factor (RF): Positive in ~80% of RA cases
-
Anti-CCP (Cyclic Citrullinated Peptide Antibody): More specific to RA and often indicates more severe disease
-
Erythrocyte Sedimentation Rate (ESR): Measures inflammation levels
-
C-reactive Protein (CRP): Another inflammation marker
-
Antinuclear Antibody (ANA): Can indicate other autoimmune conditions that sometimes overlap with RA
Why Proper Diagnosis Matters
A correct and early diagnosis is critical to:
-
Starting effective treatment
-
Preventing joint damage and disability
-
Improving long-term quality of life
Because RA and OA have different causes and treatments, identifying the correct condition ensures the most appropriate care plan.
RA vs. OA: Prognosis
Both Rheumatoid Arthritis (RA) and Osteoarthritis (OA) are chronic conditions, meaning they last a lifetime. Neither disease currently has a known cure, but their long-term outlooks—or prognoses—differ significantly.
Osteoarthritis (OA) – Predictable but Progressive
OA is a degenerative joint disease that gradually worsens over time. The rate of progression can vary from person to person, but it’s generally more predictable than RA.
With appropriate treatment and lifestyle changes:
-
Joint pain and stiffness can be managed
-
Mobility and quality of life can be preserved
-
Progression may be slowed
OA does not typically affect other organs or systems, making its overall prognosis more stable and positive, especially with early intervention.
Rheumatoid Arthritis (RA) – Unpredictable and Systemic
RA is an autoimmune disorder that causes chronic inflammation and can affect multiple organs, not just the joints. Its progression is often less predictable than OA and may vary significantly between individuals.
Potential complications of RA include:
-
Lung problems (e.g., interstitial lung disease)
-
Heart disease
-
Eye inflammation
-
Fatigue and severe joint deformities
-
Increased risk of other autoimmune conditions like lupus
-
Higher risk of certain cancers, such as lymphoma
Because of its systemic nature and potential for serious complications, the prognosis for RA is more complex and depends on how early it’s diagnosed and how well it’s managed.
Summary Table – RA vs. OA Prognosis
| Factor | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Disease Nature | Degenerative | Autoimmune and inflammatory |
| Progression | Gradual and predictable | Variable and unpredictable |
| Affects Only Joints? | Primarily joints | Joints + other organs (systemic) |
| Potential Complications | Joint damage, mobility issues | Heart, lungs, eyes, immune system, and cancer risk |
| Prognosis with Treatment | Generally positive | Depends on the severity and treatment response |
Summary
While OA tends to have a more manageable and localized progression, RA is a more aggressive and systemic condition with a wide range of potential complications. However, early diagnosis and targeted treatment can significantly improve the outcome for both diseases.
If you suspect you may have arthritis, seeking medical evaluation early is key to preserving your health and quality of life.
Treatments for Osteoarthritis vs. Rheumatoid Arthritis
While Osteoarthritis (OA) and Rheumatoid Arthritis (RA) both affect the joints, their treatment strategies are very different due to their distinct causes. OA is mechanical and degenerative, while RA is autoimmune and inflammatory.
Osteoarthritis (OA) – Focus on Pain Relief & Joint Function
OA treatment aims to reduce pain, improve joint mobility, and maintain quality of life. It does not target the immune system, as OA is not inflammatory in nature, unlike RA.
Common OA Treatments:
-
NSAIDs (e.g., ibuprofen, naproxen) – Reduce pain and mild inflammation
-
Analgesics (e.g., acetaminophen) – Relieve pain without addressing inflammation
Non-Medication Therapies:
-
Physical therapy – Strengthens muscles and improves joint stability
-
Joint support/bracing – Offloads stress from affected joints
-
Heat and rest – Reduce stiffness and ease discomfort
-
Massage therapy & acupuncture – Alternative methods for pain relief
-
Weight management – Reduces pressure on weight-bearing joints
Rheumatoid Arthritis (RA) – Targeting the Immune System
RA treatment focuses on reducing inflammation, suppressing abnormal immune activity, and preventing joint damage. Early and aggressive treatment can slow disease progression and reduce long-term disability.
Primary RA Medications:
| Drug Type | Purpose |
|---|---|
| DMARDs (e.g., methotrexate) | Slow disease progression, prevent joint damage |
| Biologics (e.g., Humira, Enbrel, Remicade) | Target specific immune responses |
| JAK Inhibitors (e.g., tofacitinib) | Block pathways that trigger immune system inflammation |
| Corticosteroids (e.g., prednisone) | Rapidly reduce inflammation and flare symptoms |
| NSAIDs & Analgesics | Provide symptom relief, but do not stop disease progression |
Steroid injections may be used in both RA and OA for short-term relief of localized joint inflammation and pain.
Shared Treatment Strategies for RA & OA
-
Weight Management:
Helps reduce joint stress in OA and can also reduce systemic inflammation in RA. -
Surgical Options (if needed):
-
Arthroscopy – Removes loose cartilage or bone fragments
-
Arthrodesis (joint fusion) – Stabilizes or relieves pain in smaller joints
-
Arthroplasty (joint replacement) – Most common in hips, knees, and shoulders
-
Summary
While OA treatments center around joint support and pain relief, RA management targets the immune system and inflammation to prevent permanent joint damage. Both conditions benefit from a multidisciplinary approach that may include medication, therapy, lifestyle modifications, and, when necessary, surgical intervention.
If you suspect you have arthritis, working closely with a rheumatologist or an orthopedic specialist ensures that you receive the right diagnosis and treatment tailored to your specific condition.
Sources Link
https://www.ncbi.nlm.nih.gov/books/NBK441999/
https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
https://www.health.harvard.edu/pain/explain-the-pain–is-it-osteoarthritis-or-rheumatoid-arthritis